This knowledge base article will provide guidance on how to successfully access and bill for your monthly Remote Patient Monitoring and Chronic Care Management billing report.
Accessing Billing Reports (Expect to see your billing reports uploaded by the 1st week of every month)
1. Go to rpm.evelyn.one
2. Click on the first of the 3 orange icons at the top right of the Patient Overview dashboard that looks like a file:
3. DO NOT re-enter your credentials; simply click on the red button toward the bottom that says "Sign in with Auth0"
4. You will see your monthly reports titled: "Accuhealth Medicare Revenue Report - RPM and CCM - Clinic Name - December 2022;" click on the report you would like to download and then click on the red download button in the top right corner:
**this will download into an excel spreadsheet:
5. Once report is downloaded, you will be able to open the fields to access all data necessary for billing, including Dates of service to bill for RPM and/or CCM services. Most patients receiving accuhealth services may have eligible billing codes for both RPM and CCM (Note - if your clinic is not participating in CCM Services you are encouraged to email success@accuhealth.tech for more information), for which the CPT codes can and should be included in the same claim when they share the same Date of Service.
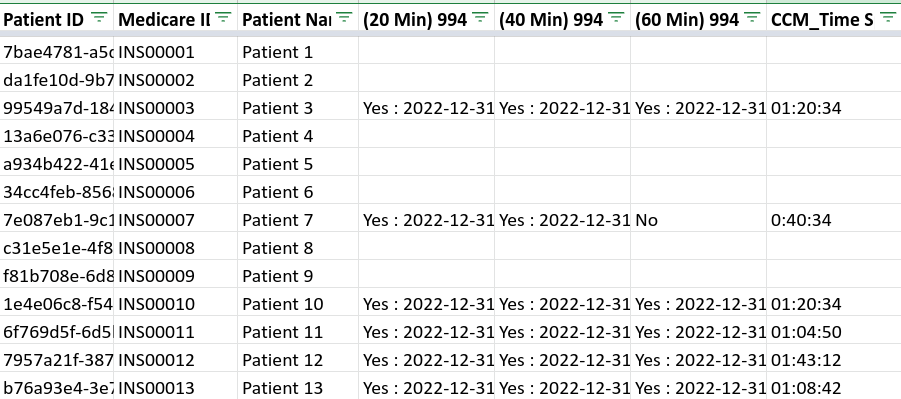
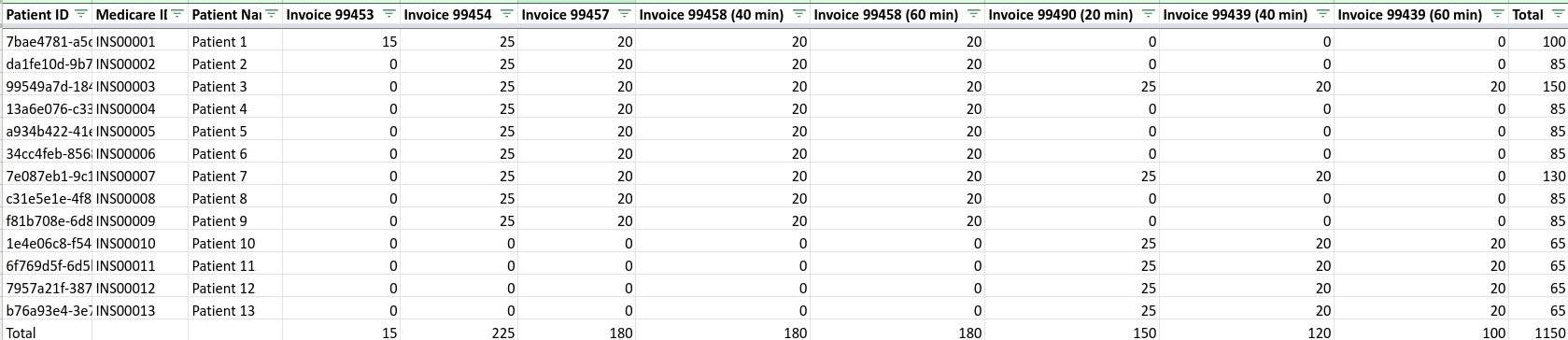
The Billing Report is structured in the following groups:
a) Patient and Provider Demographics
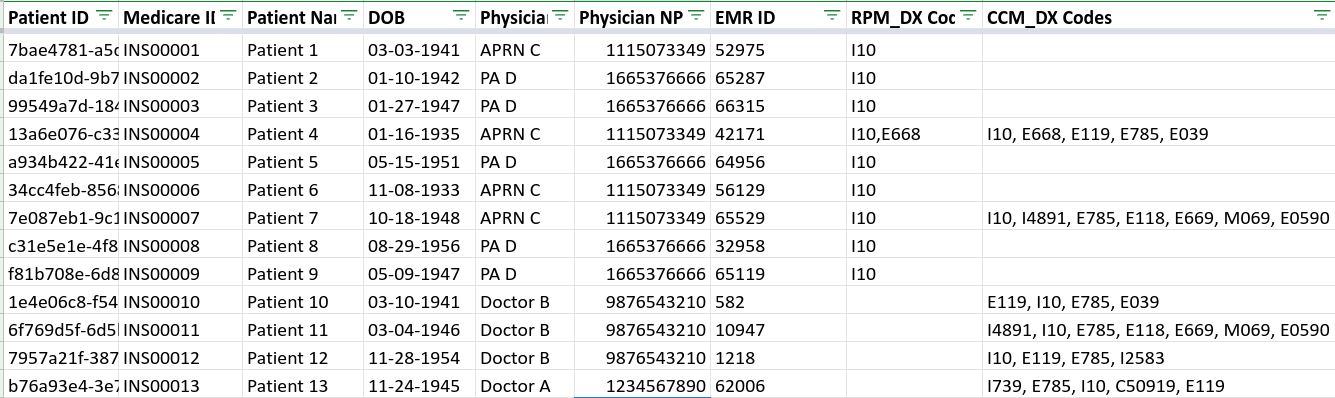
b) Remote Patient Monitoring Codes and Dates of Service
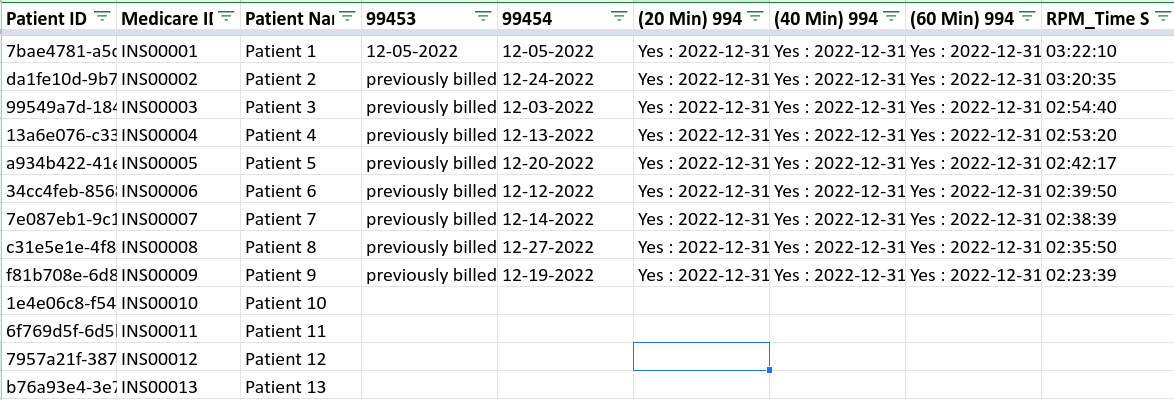
c) Chronic Care Management Codes and Dates of Service
d) Invoicing per CPT Code of Accuhealth Services Rendered
How to bill for each CPT code
RPM CPT Codes
1. 99453 - This code is billed one time only for the initial set-up of the patient.
2. 99454 - This code is billed every 30 days for the patient have a functioning device that synchronously transmits data to the referring provider. This code requires that the patient successfully transmits data for a given number of days within a 30 day period.
3. 99457 - This code is billed monthly (last day of the month) for the first 20 minutes of interactive time spent with a patient.
4. 99458 - This code can be billed for up to 2 units, which is for an additional 20 minute block of time spent with a patient (for a total of 1 hour of time spent). Your billing report will conveniently have the 99458 (40 min) and 99458 (60 min) in separate columns to clearly illustrate if the code requires 0, 1, or 2 units.
CCM CPT Codes
5. 99490 - This code is billed monthly (last day of the month) for the first 20 minutes of interactive time spent with a patient for Chronic Care Management services.
6. 99439 - This code can be billed for up to 2 units, which is for an additional 20 minute block of time spent with a patient (for a total of 1 hour of time spent). Your billing report will conveniently have the 99439 (40 min) and 99439 (60 min) in separate columns to clearly illustrate if the code requires 0, 1, or 2 units.
**Please be sure to follow the dates of service provided to you in the monthly billing reports for each code.
How to drop claims in your EMR (We only auto-generate claims for Athena clients)
1. Claims should include all CPT codes that share the same date of service - RPM and CCM codes can and should be included in the same claim when they share the same date of service (i.e. RPM Interactive Time codes 99457 and 99458 should be included in the same claim as CCM Interactive Time codes 99490 and 99439 as they will always share the same date of service - the last day of the respective calendar month)
2. In the claim, make sure to include the diagnosis code(s), the Place of Service as 11, and the number of units. Note that the number of units will always be one for every code, except 99458 and 99439. This code can be billed for up to 2 units max.
3. CCM codes require a minimum of two (2) diagnosis codes associated to CPT codes 99490 and 99439. Please note many CCM patients have many diagnosis codes being treated, you only need to include two of the codes in the claim.
Accuhealth does not provide billing advice. Each provider is responsible for the accuracy and validity of their own charges
